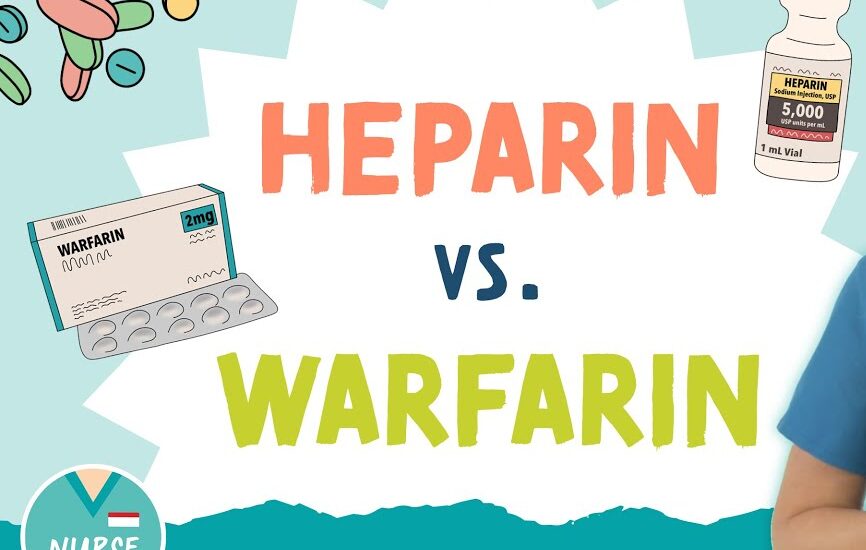
Heparin and warfarin are two of the most used anticoagulant medications in clinical practice. These drugs prevent and treat thromboembolic events, such as deep vein thrombosis (DVT), pulmonary embolism (PE), and atrial fibrillation. However, they both have different mechanisms of action, pharmacokinetics, pharmacodynamics, and monitoring requirements.
In this article Heparin vs Warfarin , we will compare these two drugs by explaining their key differences and similarities, including their pharmacokinetic and pharmacodynamic properties. Additionally, we will highlight the drug of choice for different conditions, and also the antidotes of both heparin and warfarin.
Popular Brands of Heparin
- Heparin (Unfractionated Heparin)
- Heparin Sodium (generic)
- Hep-Lock
- Liquaemin
Popular Brands of Warfarin
- Warfarin Sodium (generic)
- Coumadin
- Jantoven
- Marevan
Comparison of Heparin vs Warfarin
| Parameter | Heparin | Warfarin |
| Mechanism of Action | Inhibits thrombin and factor Xa, preventing fibrin formation | Inhibits vitamin K epoxide reductase, decreasing clotting factors (II, VII, IX, X) |
| Route of Administration | Intravenous (IV), subcutaneous (SC) | Oral (PO) |
| Onset of Action | Rapid (within minutes, IV) | Slow (takes several days to reach therapeutic effect) |
| Half-life | Short (1–2 hours) | Longer (20–60 hours) |
| Monitoring | Requires regular monitoring (aPTT or anti-Xa assay) | Requires regular monitoring (INR) |
| Reversal Agent | Protamine sulfate | Vitamin K or fresh frozen plasma (FFP) |
| Pharmacokinetics (Absorption) | Not absorbed orally, must be injected or infused | Well absorbed from the gastrointestinal tract |
| Pharmacokinetics (Distribution) | Rapidly distributes in the bloodstream, does not cross the placenta | Extensively bound to plasma proteins, crosses the placenta |
| Pharmacodynamics | Immediate anticoagulant effect, short duration | Slower anticoagulant effect, longer duration |
| Indications | Acute situations like DVT, PE, and during surgeries | Long-term anticoagulation for prevention and treatment of DVT, PE, atrial fibrillation |
| Drug of Choice | Initial therapy for acute thromboembolic conditions | Long-term anticoagulation management or chronic use |
| Major Side Effects | Bleeding, heparin-induced thrombocytopenia (HIT) | Bleeding, skin necrosis, teratogenicity (during pregnancy) |
Drug of Choice for Different Conditions – Heparin vs Warfarin
Heparin
Heparin is preferred for acute thromboembolic conditions, where immediate anticoagulation is necessary.
These conditions include:
- Acute Pulmonary Embolism (PE)
- Deep Vein Thrombosis (DVT)
- Myocardial Infarction (MI)
- Surgical Procedures (e.g., during heart surgery or orthopedic procedures)
Heparin is effective in emergency settings when rapid anticoagulation is required. Additionally, it is used as a bridge therapy when transitioning from one anticoagulant to another.
Warfarin
In chronic conditions, Warfarin is the drug of choice for long-term anticoagulation management.
- Atrial Fibrillation (AF)
- Mechanical Heart Valves
- Chronic Venous Thromboembolism (VTE)
- Stroke Prevention in patients with AF
Because warfarin’s effects take time to develop and its anticoagulation also lasts for a longer period, it is the better choice for long-term management.
Heparin Antidote
The antidot of Heparin is Protamine Sulfate.
- Mechanism
Protamine sulfate is a positively charged peptide that binds to heparin, neutralizing its anticoagulant effect. It works by forming a stable complex with heparin, thereby reversing its ability to inhibit clotting factors.
- Usage
Protamine sulfate is commonly used in cases of heparin overdose or when rapid reversal of heparin’s anticoagulant effect is needed, such as during surgery or in cases of major bleeding.
- Dosing
The dose of protamine depends on the amount of heparin administered, the general guideline is to administer 1 mg of protamine for every 100 units of heparin given in the past 30 minutes for unfractionated heparin
Warfarin Antidotes
Vitamin K (Phytonadione)
- Mechanism: Vitamin K directly reverses warfarin’s anticoagulant effect by promoting the synthesis of clotting factors (II, VII, IX, and X) in the liver.
- Its administration is through oral route, and intravenously in more severe cases.
- The dose of vitamin K varies depending on the severity of the warfarin toxicity.
For life-threatening bleeding
- we require higher doses (5–10 mg IV)
- oral administration (1–2 mg) in less urgent situations.
Fresh Frozen Plasma (FFP) or Prothrombin Complex Concentrates (PCCs):
- FFP and PCCs contain clotting factors that have been depleted by warfarin, providing a rapid way to restore clotting function.
- These are used in severe bleeding cases or when an immediate reversal is needed.
Conclusion
Heparin and warfarin are both important anticoagulants in the management of thromboembolic disorders, but they have different properties that make them suitable for different situations. Heparin’s rapid action and short duration make it ideal for acute settings, while warfarin’s long-term effects are more appropriate for chronic anticoagulation therapy.